Breastfeeding after Reduction
My original intention was to revamp old breastfeeding blogs after reviewing them.
I can’t do that. I’m honoring who I was when I wrote the original blogs, and I need to write another one honoring the growth and wisdom I have gleaned since those experiences.
Recap if you’re new around here:
I had a breast reduction at the age of 12.
I was it 36 DD and simple existing was very uncomfortable.
I would go to sleep crying because of how sore my shoulders and back were at the end of the day.
My breasts didn’t come by happenstance. My family never had a healthy relationship with food, and seldom ate food in its original form. I was always active until it got to the point where running became painful from the literal weight on my shoulders.
Knowing what I know now I would’ve taken many different routes and avoided cosmetic surgery.
(more on this in the resource section below)
Another important note, at this age, the eating disorder that I have shared about previously was starting to take deeper roots. The freedom that the reduction provided helped me be more active, which made my weight loss even more significant and FAST, which led to more “positive” attention, which continued to attribute to feeding my ego of being small. My binging and purging would continue for years after the reduction.
I can’t go back and change what I did, it’s in the past.
I’m addressing this because, in the previous blog posts, I stated that I would do it all again and I can’t say that now knowing what I know.
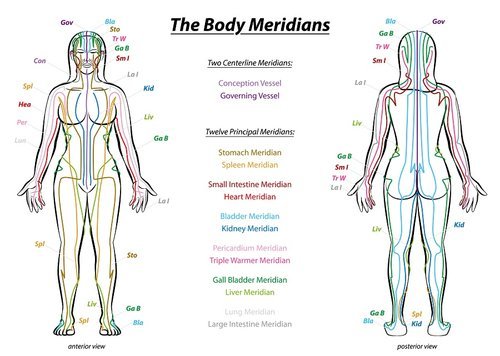
Below is a visual representation of The Body Meridians. Look closely and see how many of these run over and or through where incisions are made with these two common styles of breast reduction. (I had the anchor-pattern breast reduction.)
the breasts hold so much energy!
It’s no coincidence that I have had digestive issues ever since my surgery, and I know the two are not separate from each other.
what I’ve mentioned in a previous blog post is going into my surgery at 12 my initial question during the consultation was will I be able to breastfeed. Yes, at 12 I knew I wanted to breastfeed my children and at 12 I had concerns, or I knew instinctively that it could potentially affect my breast-feeding relationship with my future children. The surgeon assured me multiple times in multiple different ways that yes I would absolutely be able to breastfeed with no problem. (50% of women are able to breastfeed after a reduction in some capacity. 90% of that 50% will need to supplement in some capacity.
in my lived experience, for any type of augmentation that has been done to the breast, an IBCLC is an incredibly valuable resource. Yes, IBCLCs are valuable in general, but because there’s been tissue damage, scar tissue, and a change in the layout and makeup of the breast tissue, having somebody who has extensive training on breastfeeding is an invaluable resource to help with breastfeeding in any capacity.
I’ve had two different breastfeeding relationships between my two living children. With Evie, I was anxious and overwhelmed. I was not well supported and going into motherhood I didn’t think breastfeeding would be a problem. I was very unprepared. I had a CLC support us for one session when Evie was a day or two old. Evie successfully breastfed for 18 months. We were able to stop supplementing with formula at 6-7 months old, and it was a huge source of anxiety. She used a nipple shield for the first year due to my nipples being flat/inverted, until one day she pulled it off my breast looked at it curiously, and then threw it to the side and never looked back.
I ended up weaning her (unfortunately) cold turkey when I was pregnant with Olive due to fluctuating hormones and being overwhelmed and undersupported at 18 months postpartum. Olive was born at 10 weeks into our pregnancy and through my grief of my baby dying, I had also lost a huge part of Evie’s and my relationship.
Fast forward to Atlas and our relationship. I prepared and prepared and prepared as much for postpartum as I could while I was pregnant with him. During this preparation, I networked professionally and personally with an incredible IBCLC, and she is so much more than that!
Prenatally, I already had discussions with her. She already knew my surgery history and we were able to discuss a lot of my concerns. After Atlas was born she helped troubleshoot virtually and then I was fortunate enough that she was able to come to me for in-person support. She was able to affirm that my nipples were in fact not flat/inverted from anything other than a hormonal level. Once I had rested enough, and continued nourishing my body (through nourishing food & Milk Moon Supplements) my nipples were able to hold a firm shape for his latch. He used The Bridge only once before he had it on his own!
I didn’t have cracked or sore nipples because I was less anxious, I was well supported I was well nourished, and my anxiety was nowhere near what it was my first time.
I have since reached out to Jen numerous times for ongoing support (remember that blister ON MY NIPPLE?). Atlas is almost 3 and we still have an ongoing breastfeeding relationship which I attribute to her support and affirmation.
Some might attribute all of this to the fact that I am a second-time mom and I’ve done this before. I attribute it to that as well in some capacity. I wouldn’t have known how to prepare, I feel like those who prepare for themselves postpartum and they lay that healthy foundation of nourishment and rest are less likely to run into a lot of avoidable circumstances.
There’s little room for pathological diagnoses because physiologically we’re being tended to. We’re being nourished with healthy food to help and support our nervous system. We’re sleeping and resting. Yes, we are waking up to feed our children that wake up every couple of hours, and we’re physiologically being tended to in a way that we were designed to, there’s little to no room for depletion (which manifests as anxiety and depression).
Here are my resources:
Find an IBCLC or an INNATE Postpartum Care Certified Practitioner in your area who is well-versed in postpartum care to help you prepare for postpartum and other helpful products that you might want to use in support of your breastfeeding journey!
The Lactation Loop: Located in multiple states, and provides virtual support!
INNATE Postpartum Care Practitioners Directory
Items/ Supplements:
Milk Moon Supplements: Bring Me a Dream and the Postpartum Tonic are my favorites! “AUDREY” to save 10% off your order!
Haakka - cherish every magical drop
Books:
Defining Your Own Success: Breastfeeding After Breast Reduction Surgery
The Womanly Art of Breastfeeding
7 Times a Woman -I’ve been implementing the information from this book for the past 3 years. Specifically with breast health. If you are a woman or have a daughter this book is an incredible resource!
This is specifically written from my perspective of having breast augmentation. If you have not had augmentation, an IBCLC can still be beneficial, or support can be as simple as spending time while you’re pregnant with other mothers who are currently breastfeeding. Join your local La Leche League, or simply observe other mothers in the wild breastfeeding their babies! This is why it is so important for us as breastfeeding mothers to DROP THE COVER!
A few breast-feeding facts:
the world national average for breast-feeding age is 2 1/2
most women in the United States don’t breastfeed past two weeks.
Breastmilk is made up of our blood, which means we’re constantly in a state of “bleeding” and cool, and as long as we are breastfeeding our qi is being “leaked” based on TCM.
it takes 30% of our physical energy to make breastmilk (our brain uses 20% of our physical energy to put things into perspective)
*This post contains affiliate links with companies and or products that I LOVE, and I make a small commission off of purchases made using my link and or code at no additional cost to you.